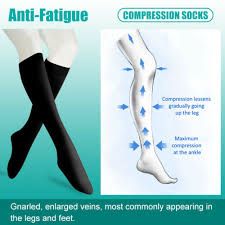
Compression Socks 20-30 mmHg is a form of Graduated compression sock that ensures that pressure is applied at a particular level on your leg. The greatest compression is often near the ankle, and it reduces further up the leg. This helps to push blood back to the heart from the leg in order to enhance blood circulation and relieve pain caused by poor circulation. The best compression stockings for you is the one that has the perfect compression levels to improve your condition. Of all the compression levels, 20-30 mmHg happens to be the most common. Read on to find out why.
Compression Gear 20-30 mmHg

Compression socks 20-30mmHg are the most commonly prescribed compression level. Often called Firm Compression or Class I, compression gear 20-30mmHg can come in any of the compression sock styles such as knee length, thigh length, and waist length styles. They can also be found in different patterns and colors to make you look fashionable while treating your medical condition.

Doctors prescribe 20-30mmHg compression stockings for preventing and treating venous disorders by promoting the flow of venous blood. They are also prescribed for preventing and relieving painful symptoms of these venous disorders.

Why Compression Matters with Compression Stockings 20-30 mmHg

Compression socks 20-30 mmHg are the most popular for treating medical conditions. Here are some of the major medical conditions that using compression stockings 20-30 mmHg can help prevent and manage.
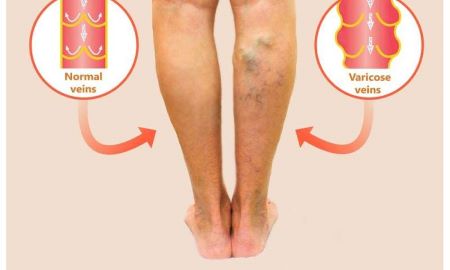
Compression socks help in preventing and relieving moderate to severe varicose veins
Veins are known to carry blood that has low oxygen content from a person’s body to the lungs and the heart. When these veins are unable to properly circulate the blood, they will bulge with blood and become visible. These enlarged, twisted veins are called varicose veins and can develop on any part of the body, but often in the thighs and legs.

Large varicose veins are often visible, long, bulging, dilated to more than 4mm in diameter and can be felt by touching. Small spider veins, also called telangiectasias, can also appear on the surface of the skin, and often look like fine, short lines, web-like maze, or starburst clusters. Spider veins are not palpable and are often found in the feet, ankles, and thighs.

Risk factors and causes of varicose veins: Varicose and spider veins are not really gender-specific but usually appear in seniors and women in childbearing their years. The risk factors include:
- blood clots or obstructions in the veins
- diseases, such as congenital abnormalities in the veins
- genetics
- phlebitis
- pregnancy
- prolonged standing
- sedentary lifestyle
- weight gain

Symptoms and complications of moderate to severe varicose veins: Symptoms of moderate varicose veins may include:
- color changes
- rash
- sensations like aching, burning, or a heavy feeling in the legs
- sores on the legs

When they get severe, they will produce long term swelling that may lead to more serious problems of the skin and tissues like nonhealing sores and ulcers. If varicose veins become complicated, they can lead to ulcers, bleeding, and blood clots.
Prevention of varicose veins: to prevent varicose veins:
- do not cross your legs while sitting
- do not wear tight clothing
- exercise regularly
- maintain a healthy weight
- put your feet up while sitting
Treatment of varicose veins: There are many treatment options for varicose veins, often depending on the size, location, symptoms, and skin changes. Medical treatment for cases of moderate to severe varicose veins include:
- elevation of the legs for about 15 minutes 4 times a daily
- micro-phlebectomy
- sclerotherapy
- thermal ablation
- vein stripping
- compression socks
How can 20-30mmHg compression socks help varicose veins?
One of the easiest methods for preventing and treating varicose veins is wearing compression stocking 20-30mmHg. Compression Socks with this pressure gradient are very popular (similar to how popular the rose toy https://comprogear.com/rose-toy/ is lately). The pressure from them will compress the arteries and veins on the leg surface. This will help your circulatory system to easily move deoxygenated blood back to your heart.

Recent studies found that wearing 20-30 mmHg stockings every day for up to six months can help reduce the aches and pains that are associated with varicose veins. For pregnant women with varicose veins who are dealing with leg swelling, these compression gear help to control the swelling and other discomforts. Even if you have not noticed any symptom of varicose veins, use compression stockings during pregnancy, long air or road trips, and if you spend a lot of time standing or sitting.

Compression socks help to treat moderate to severe edema or lymphatic edema
Lymphatic edema is the result of accumulation of lymphatic fluid in the arms and legs that causes swelling. Edema is the general reaction of your body to injury or inflammation and can develop in a small part or in your entire body. When small blood vessels start to leak, they release fluid into tissues that are near them. This accumulation of fluid causes the tissues to well, and this swelling is medically referred to as edema.
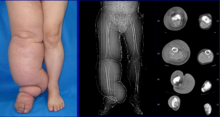
Lymphatic edema is quite different from edema caused by venous insufficiency. However, if left untreated, venous insufficiency can result in venous/lymphatic disorder.

Risk factors and causes of moderate to severe edema or lymphatic edema
Factors that tend to increase the risk of developing lymphatic edema include old age, obesity, and rheumatoid or psoriatic arthritis. Some of the causes of edema include:
- allergic reactions
- congestive heart failure (cardiovascular disease)
- disorders in the balance of substances present in the blood
- kidney disease (nephrotic syndrome)
- liver disease (cirrhosis)
- low albumin (hypo)
- obstruction in blood flow
- physical inactivity
- pregnancy
- sitting or standing for long

Edema that occurs in the leg is usually caused by:
- a cyst or tumor
- blood clot
- infection or inflammation
- lymphatic edema
- varicose veins
Primary lymphatic edema occurs on its own and can be noticed at birth or may develop much later. Secondary lymphatic edema, on the other hand, is caused by surgery or some medical treatments. For instance, breast or abdominal surgery and surgical removal of tumors and adjacent lymph nodes and vessels blocking lymph fluid from flowing freely and naturally through its system. Other surgeries like those performed for melanoma (skin cancer), bladder or colon cancer prostate or testicular cancer, and other surgeries requiring removal of the lymph node can also cause secondary lymphatic edema.

Related Articles
- Sock Soothers
- Medical Compression Socks
- Compression Socks for Men
- Best Compression Socks for Swelling
- Wide Calf Compression Socks
- Can You Wear Compression Stockings 24 Hours a Day
- Toeless Compression Socks
- Easy To Put On Compression Socks for Elderly
- Do Compression Socks Help Gout
Symptoms and complications of moderate to severe edema or lymphatic edema
Early manifestations of lymphatic edema include soft tissue swelling and edema. Progression of the disorder will result in:
- dermal thickening
- discoloration and some other skin changes
- hyperkeratosis
- papillomatosis
- ulcers
- verrucous or wart-like hyperplasia
- worsening edema

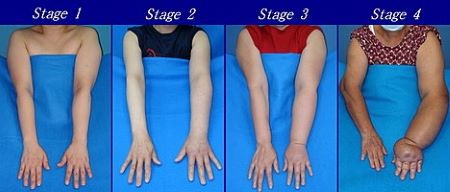
Lymphatic edema is a chronic medical condition that usually starts with mild swelling in the feet or hands. If diagnosed and treated early, its condition and prognosis can be improved. If left untreated, however, the limbs may become more edematous, causing the skin to lose its elasticity (fibrosis). This will consequently lead to infection and some irreversible complications. Lymphatic edema can also lead to cellulitis, lymphadenitis, lymphangitis, and in rare cases, a form of cancer known as lymphangiosarcoma.

Complications of lymphatic edema can result in psychological distress due to poor body image from disfiguring. It can also make it difficult for the patient to engage in activities of daily living and may require occupational therapy.
Prevention of edema or lymphatic edema
After cancer surgery involving your lymph vessels or lymph nodes, you are at risk of developing lymphatic edema. To prevent or reduce this risk:
- avoid injury to the affected limb
- rest your leg or arm while recovering from cancer treatment
- avoid heat or extreme temperatures on your arm or leg
- avoid tight clothing
- keep your leg or arm clean
- keep your leg or arm elevated.

Treatment of edema or lymphatic edema
Treatment of lymphatic edema depends on the severity of the edema and degree of fibrosis. To help with this fluid retention problem, the doctor may suggest that you do the following:
- avoid extreme temperatures
- complete decongestive therapy (CDT)
- consume less salt
- do not sit or stand for too long
- engage in regular physical activity
- exercise
- improve circulation by raising the legs a couple of times a day
- lose weight (for heavy patients)
- massage
- pneumatic compression
- surgery
- wrap your leg or arm
- wearing compression garments

How can socks 20-30mmHg help edema or lymphatic edema?
The basis for treating lymphatic edema is compression, since compression must be applied to the affected limb to lessen the swelling. Compression socks 20-30 mmHg can help by applying firm but gentle pressure to the area, thereby encouraging the lymph fluid to flow back into the bloodstream. They are comfortable, easy to use, cost effective, and lightweight. Your doctor will help you to get a correct fit.

If, however, you are finding it difficult to put on or take off your 20 30 mmHg compression socks, your lymphatic edema therapist can help you review the different aids and techniques you can use. There are different forms of compression therapy you can consider depending on the severity of your condition.

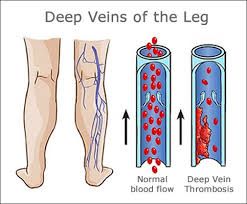
Compression socks help to prevent deep vein thrombosis (DVT) or economy class syndrome
Deep vein thrombosis (DVT) is a condition that results from the formation of blood clots in veins inside your body.

These clots can form in any part of the body, but is often found in the lower legs and thighs. DVT is a potentially life-threatening condition because there is the likelihood of a blood clot traveling to the lungs and blocking an artery, resulting in pulmonary embolism. DVT causes pain and swelling. It can occur after sitting still for too long at work or when traveling by bus, train, or air.
Risk factors and causes of deep vein thrombosis (DVT): Although deep vein thrombosis can happen to anyone, people who have just gone through a surgery in the pelvic region, tummy, or legs are at greater risk of developing it. Your risk of having DVT is higher than average if you:
- are overweight
- are pregnant or 6 weeks after putting to bed
- had trauma
- have a history of pulmonary embolism or DVT
- have cancer
- have had a stroke
- have heart disease
- have inherited tendency to having blood clots
- take medicines containing oestrogen.

Symptoms and complications of deep vein thrombosis (DVT): Symptoms of deep vein thrombosis include:
- discoloration of skin
- enlargement of superficial veins in the affected arm or leg
- skin may feel warm when touched
- swelling
- tenderness or pain in the leg when standing or walking

These symptoms are easier to recognize after taking a long trip, experiencing trauma, or just had surgery.
Prevention of deep vein thrombosis (DVT): The best preventive measure for DVT is compression stockings 20-30 mmHg. You can choose either knee-high, thigh-high, or full-length compression stockings, depending on where you are more prone to the swelling. The right compression level will guarantee faster results. If you are at risk of having DVT, wear these socks first thing in the morning and only take them off at night or when you want to take a bath.

To also help prevent DVT:
- engage in exercise
- drink plenty of water
- wear clothes that are loose and comfortable
- do not stay in one condition for too long
- avoid taking sleeping pills when traveling.
Treatment of deep vein thrombosis (DVT): After being diagnosed with DVT, you can wear compression gear to help reduce some of the swelling and general discomfort.

How can compression stockings 20-30mmHg help deep vein thrombosis (DVT)? Compression gear 20-30mmHg are usually prescribed for prevention of DVT because they help apply pressure to the legs to stop pooling and clotting of blood. These socks are made of elastic fabric that fit snugly around the ankles, legs, and thighs. They create pressure which helps to push fluid up the leg, thereby allowing free flow of blood from the legs back to the heart. Additionally, compression socks help to improve blood flow, reduce swelling, and also reduce pain in the lower extremities.

20 30 mmhg compression stockings help to provide relieve from superficial thrombophlebitis
Thrombophlebitis is a thrombus or blood clot formed inside a vein that is inflamed. It often affects many superficial veins in the body and is more common in people with varicose veins. Meanwhile, superficial veins are veins that can easily be seen near the skin’s surface, particularly in the legs.

Therefore, superficial thrombophlebitis is an inflammatory reaction that has to do with thrombus in a vein just under the skin. It is a very self-limiting and benign condition that can also be recurrent and persistent. This condition affects more females than males. If left untreated, superficial thrombophlebitis can progress through a perforating vein that involves a deep vein, resulting in more serious conditions like Deep Vein Thrombosis and Pulmonary Embolism. An ultrasound or blood test is often used to diagnose superficial thrombophlebitis.

Risk factors and causes of superficial thrombophlebitis: Some of the common risk factors of superficial thrombophlebitis are:
- chemical irritation (usually from cancer treatments)
- disorders that increase clotting of blood
- infection
- medications for hormone replacement, stroke or injury that resulted in paralysis of the legs or arms
- obesity
- old age (over 60 years)
- oral contraceptives
- pregnancy
- prolonged sitting or lying down (especially when traveling)
- recent catheter, IV, or injection into the vein
- smoking
- varicose veins
Symptoms and complications of superficial thrombophlebitis

Symptoms of thrombophlebitis include:
- coughing up blood
- pain in the limb
- red, tender, or swollen vein
- shortness of breath
- skin darkening over the affected vein
- tenderness and pain that gets worse with added pressure
- vein hardening
- warm skin and tissue in the affected area

Prevention of superficial thrombophlebitis: Superficial thrombophlebitis may not indicate a life-threatening problem per se, but it may be a sign of an underlying lethal condition like DVT and Pulmonary Embolism. You can prevent this condition if you do the following:

- avoid long hours of inactivity like prolonged sitting or standing
- avoid tight clothing
- elevate your legs
- exercise regularly
- quit smoking
- stay hydrated
- always wear compression gear when traveling long distance

Treatment of superficial thrombophlebitis: Treatment options for superficial thrombophlebitis include:
- applying heat to the affected area
- blood-thinning medications
- clot-dissolving medications
- elevating the affected leg
- filter
- using over-the-counter nonsteroidal anti-inflammatory drugs
- varicose vein stripping
- wearing compression stockings 20-30mmHg.

How can compression stockings 20-30mmHg help superficial thrombophlebitis? You can wear compression socks to treat superficial thrombophlebitis and ultimately optimize your leg health. These stockings apply pressure on your legs to improve blood flow and help to reduce swelling in the affected area. When you wear these prescription-strength socks, they will help to alleviate swelling and pain in your legs, and also reduces chances of complications like DVT. There are many lightweight, comfortable, classy, medically effective, and durable compression socks 20-30 mmHg on ComproGear.com.

20 30 mmhg socks are helpful in preventing orthostatic hypotension. Also referred to as postural hypotension, Orthostatic Hypotension occurs when there is an unexpected drop in blood pressure caused by posture change, like when a person quickly stands up.
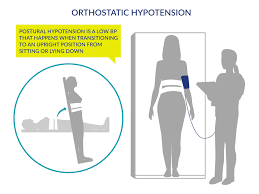
Orthostatic hypotension, which is a problem that is common in older people, is associated with increase in falls, cognitive impairment, cardiovascular disease, stroke, and mortality.
Risk factors and causes of orthostatic hypotension: Causes of orthostatic hypotension are:
- anemia or low red blood count
- heart conditions like valve disease and irregular heart rhythms
- loss of fluid within blood vessels
- Parkinson’s disease
- pregnancy
- some medications like antidepressants and beta-blockers

Symptoms and complications of orthostatic hypotension: Losing consciousness is a common complication of this condition.
- blurred vision
- dizziness
- fainting
- falling
- fatigue
- light-headedness
- nausea

Treatment and prevention of orthostatic hypotension: Some of the ways you can prevent or manage orthostatic hypotension include:
- avoid or reduce alcohol intake
- avoid strenuous activity when the weather is hot
- elevate the head of your bed slightly when sleeping
- include salt in your meals
- stay hydrated by drinking plenty water
- when you are getting out of bed, sit on the edge for a minute before you stand
- use compression sock 20-30mmHg
How can socks 20-30mmHg help orthostatic hypotension? Wearing waist-high compression stockings 20-30mmHg can help promote circulation of fluid and prevent them from pooling in your legs. They will reduce the symptoms of this condition and also prevent its reoccurrence. Wear them during the day and take them off only when you want to lie down at night.

Conclusion
This article looks into why compression matters and concentrates on compression level 20-30 mmHg. Compression socks with this compression level is the perfect tool to use if you want to improve and relieve some medical conditions.
This page last updated January 24, 2022
