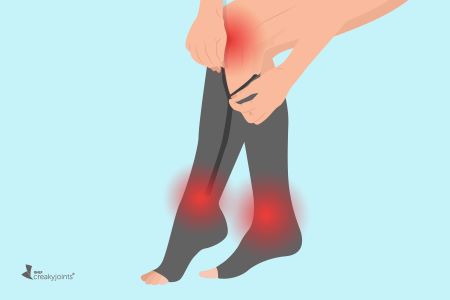
You’ve been doing it since you were a small child and have probably gotten fairly good at it by now–so why do you need to learn how to put on your socks again?! Compression socks are not the same as regular socks in that they are not just there to keep your feet warm. They provide pressure over the ankles and calves that can improve your health in a myriad of ways.
How to Safely Wear Compression Socks After Hip or Knee Replacement

If you have had hip or knee troubles, then joint replacement surgery can be liberating! When your rehab and healing are complete, you’ll likely be more active and comfortable than before surgery, but it can be a long road to get there. For elderly people who break their hips during falls, joint implants can restore their mobility.
After hip or knee replacement operations, surgeons typically prescribe compression stockings to facilitate recovery. But getting the compression socks on your legs properly is critical to healing and recovery. Putting compression socks on can be a bit tricky after surgery because you need to avoid certain movements until your new joint is stable.
Why Wear Compression Socks?
Compression socks are elastic and snug, applying gentle force to the veins in your legs. In knee-high compression socks, the tension is greatest at the ankle and tapers off through your calf. This pressure gradient fights against gravity and drives blood upward toward the heart, promoting better circulation and preventing fluid buildup in the lower legs.

Improved circulation provided by compression socks promotes healing as the oxygen and nutrients from the blood move through the operative site, speeding tissue repair. Similarly, medications disperse more efficiently, possibly giving quicker relief from pain and inflammation. Since compression socks control swelling, movement may also be easier and less painful.

Compression socks not only promote healing, but they can reduce the risk of a blood clot in the leg, which can be a side effect of being less active while recuperating. Blood clots are dangerous because, if a clot travels to an artery that feeds the heart or lungs, the blockage can be fatal if it isn’t found early.
Knowing the proper way to handle compression socks allows you to enjoy their benefits without endangering your health. Since the movement restrictions for the hip and knee vary, it is important to follow those provided by your doctor for your type of surgery.

Compression Sock Pressure Grades
High-quality compression socks vary in gradient strength, determined by their materials and weave. Their force is measured in millimeters of mercury, written as “mmHg.” Here are the four pressure grades most widely used, along with their support levels.
- 8-15 mmHg – light support
- 15-20 mmHg – medium
- 20-30 mmHg – firm
- 30-40 mmHg – extra firm
After knee and hip surgeries, most orthopedic surgeons prescribe firm compression stockings. If your doctor hasn’t specified a pressure grade, ask if they approve of knee-high socks rated 20-30 mmHg.
Compression Socks and Precautions after HIP REPLACEMENT
Generally, you’ll need to observe hip precautions for six to 12 weeks after hip surgery, but the time frame depends on how fast you heal. At a minimum, it takes around five weeks for your bones to begin to fuse with the implant. Safe positioning keeps the hardware from becoming dislocated and causing serious problems.

Dislocation Risk
The hip joint basically consists of two bones, a ball-shaped one that fits into the one shaped like a cavity or “socket.” To replace them, the surgeon must separate the muscles holding these bones together. This process overstretches the muscles, weakening them, making it easy for the new ball to slip from its socket in certain poses.

Evidence of dislocation may include:
- audible popping
- severe pain in the hip and groin
- the leg recovering from surgery is shorter than the other leg
- difficulty moving leg and/or walking

Dislocation is unwelcome because restoring the implant requires hospitalization. The restorative procedure, called a “reduction,” is performed with a patient under general anesthesia or light sedation. With a mild dislocation, a surgeon can reposition the bones without cutting any tissues. After reduction, to prevent subsequent dislocation, a brace is usually worn.

Hip Restrictions
Once your muscles regain their strength, they’ll hold your hip joint securely, making restricted movement unnecessary. Meanwhile, the precautions are critical:
- Do not cross your legs at the ankles or knees. Keep your legs about 6 inches apart.
- When seated, keep your hips slightly higher than your knees, sitting on a pillow if necessary. Avoid using low toilets, chairs, couches, and beds. Sit in chairs that have arms.
- When standing up, grasp the armrests and slide your body to the edge of the chair. Avoid leaning forward to stand. When sitting back down, try to keep the back straight.
- When sitting or lying down, don’t pull the knees toward the chest.
- While standing, don’t raise the knee above the hip that has been replaced.
- Don’t let the foot of the operated leg turn inward, whether seated, standing, or lying down. Also, keep toes pointed outward when walking.
- Don’t sleep on the side the surgery was performed on.
- Use aids that minimize bending, including a long-handled shoehorn, reacher, and Velcro shoe closures rather than laces.
Compression Socks and Precautions after KNEE REPLACEMENT
After knee replacement, dislocation is rare. Still, during the three months of post-op recovery, you’ll need to modify some activities to avoid rupturing the stitches or staples at the incision and to keep from straining the knee muscles.

Knee Restrictions
- Avoid putting on pants or socks while standing. Either sit on a chair or the edge of the bed. Do not occupy low chairs, soft chairs, sofas, rockers, or stools.
- Choose furniture with armrests since their leverage facilitates standing. The best way to exit a chair is by sliding to the edge, gripping the arms, and pushing yourself up.
- When seated, aim the knees and feet forward rather than turned inward or out.
- Never squat or jerk the leg where the knee has been replaced.
- Avoid extreme forward bending and reaching.
- Use accessories that minimize bending, including a long-handled shoehorn, reacher, and Velcro shoe closures versus laces.

How to Put On Compression Socks with a Helper
Now, let’s discuss how to put on compression socks after knee surgery or hip surgery:
It is important to note that until your doctor cancels your movement restrictions, another person must put the socks on for you.
Positioning
The best way to work with your assistant is by taking a position that doesn’t strain their back. Ideally, sit on a chair or the edge of your bed, with your legs over the side. Avoid letting your feet dangle, as they’ll likely turn inward. If your feet don’t reach the floor, place them on a footrest, or box.

Turning a stocking inside out makes it easier to manage. To do this, your helper should hold their palm up and slide their arm through the back of the hose, until they grasp the heel. Next, they should tuck the heel under their thumb, resembling a sock puppet. Still holding the heel, the helper should pull the sock down and over their arm. With the toe right-side out, they can slide the hose off their arm and turn it over.

Holding your foot straight, your helper should place the sock on your toes and then roll it halfway up your foot. (At this point, they may apply rubber gloves to help with gripping.) Then, they should slide the rest of the sock up your calf and leg so that the stocking ends two finger-widths below the knee. After your assistant straightens the hose, they should smooth the fabric with their palms. Repeat the process for the other leg.
Note: Before dressing further, make sure the fabric is free of wrinkles, bunching, and folds as this can impede your circulation. For the same reason, never cuff the top of the stocking.
Sock Removal
Taking compression socks off is easy with a helper. With both hands, your helper should grip the top of the stocking and slide it down over the leg, inside out. After pulling the hose over your heel and supporting your calf, your helper should be able to easily slip the sock off your foot.
How to Put On Compression Socks By Yourself
Once your doctor lifts the movement restrictions, you can apply the stockings independently. With this milestone, your healing is well underway! However, even after a full recovery, you should still avoid extreme bending.

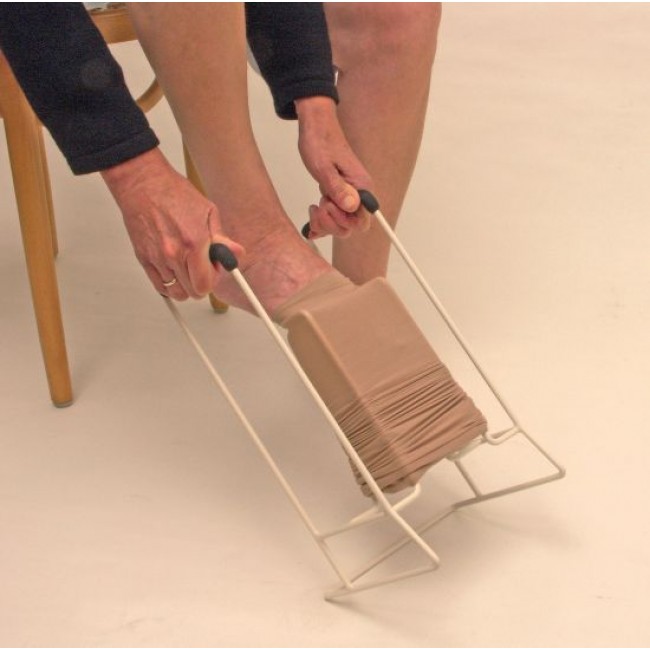
To make wearing compression socks easier, an array of clever gadgets are available. You’ll find them at surgical supply stores and online, sold as “donning and doffing aids.” Your physical therapist can likely recommend a particular design or brand that’s ideal for you. Here are two examples, along with video demos and links to sellers:
Medi Butler – This is an upright metal frame with a stirrup in the center that holds the sock inside out, stretching it open. First, slide the stocking over the stirrup until you see the heel pocket. After placing your foot inside the sock, step onto the floor and pull the frame toward you.

The Mediven Butler Off streamlines hose removal. It consists of a long aluminum rod with a shoehorn-like device at one end and a plastic handle at the other. Hook the horn on the back of your stocking and slide it along your skin. Upon reaching your ankle, point your toes down. Then, push the horn toward your toes and slip off the sock.
Wearing Compression Socks to Control Swelling
After both hip and knee replacements, swelling around the incision is normal. Additionally, fluid may accumulate in the ankle and foot on the joint-replacement side. This swelling or “edema” can persist for several weeks to months, particularly after knee surgery. While elastic compression stockings can be open toe or closed toe, differing by whether fabric covers the whole foot, closed-toe styles are best for foot edema. Since open toe socks don’t support the foot as well, any postoperative swelling may worse.

Typically, edema is lowest in the morning because leg elevation during sleep directs the blood toward your heart. Applying compression socks is the easiest and most effective first thing in the morning. Remove the hose at bedtime, unless your doctor instructs otherwise. Continue daily wear until edema resolves.
Always adhere to your doctor’s protocols for how to put on compression stockings safely.
Wearing Compression Socks
Once you can put on your compression socks, you’ll be ready to go! Wearing compression socks is a simple way to speed your recovery. Through daily use, you’ll have the possibility of better circulation, tissue mending, drug delivery, pain relief, and reduction of swelling. You’ll also cut the chances of getting a blood clot which can be dangerous or even life-threatening. Who would have thought that a pair of socks could save your life?
General Precautions
The material presented on ComproGear.com is meant to be educational, not overriding professional medical advice. Always heed the instructions of your surgeon and rehab team concerning your post-op care. If something hurts, it’s probably wrong–stop and ask your doctor or nurse for help. Double-check with your doctor or rehab specialist to make sure you’re wearing your compression socks properly as you move along the journey toward health and healing.
ComproGear Compression Socks
ComproGear sells Compression Socks that can help you through your time of recovery.
